-
Acquired Brain Injury (ABI)
-
Agnosia.
-
Alzheimer's disease.
-
Amnesia.
-
Dementia.
-
Hyperthymestic syndrome.
-
Huntington's disease.
-
Parkinson's disease.
-
Stress
-
Wernicle-Korsakoffs syndrome
-
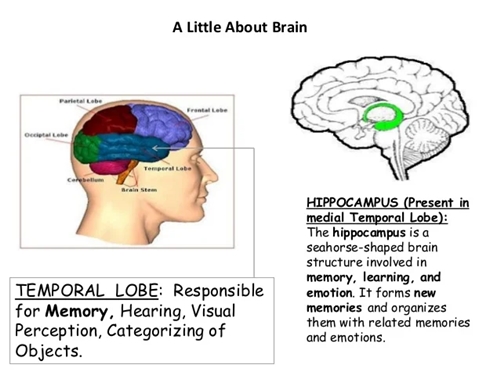
Agnosia
Agnosia is
the inability to recognize
certain objects, persons or
sounds. Agnosia is typically
caused by damage to the brain
(most commonly in the occipital
or parietal lobes) or from a
neurological disorder.
Treatments vary depending on the
location and cause of the
damage. Recovery is possible
depending on the severity of the
disorder and the severity of the
damage to the brain. Many more
specific types of agnosia
diagnoses exist, including: associative
visual agnosia, astereognosis, auditory
agnosia, auditory
verbal agnosia, prosopagnosia, simultanagnosia, topographical
disorientation, visual
agnosia etc.
-
Alzheimer's disease
Alzheimer's disease (AD)
is a progressive, degenerative
and fatal brain disease, in
which cell to cell connections
in the brain are lost.
Alzheimer's disease is the most
common form of
dementia. Globally approximately
1–5% of the population is
affected by Alzheimer's
disease. Women are
disproportionately the victims
of Alzheimer's disease, with
evidence suggesting that women
with AD display more severe
cognitive impairment relative to
age-matched males with AD, as
well as a more rapid rate of
cognitive decline.
-
Amnesia
Amnesia is
an abnormal mental state in
which memory and learning are
affected out of all proportion
to other cognitive functions in
an otherwise alert and
responsive patient. There are
two forms of amnesia: Anterograde
amnesia and retrograde
amnesia, that show hippocampal or
medial temporal
lobe damage.
Anterograde amnesics show
difficulty in the learning and
retention of information
encountered after brain damage.
Retrograde Amnesics generally
have memories spared about
personal experiences or context
independent semantic
information.
-
Brain injury
Traumatic brain injury often
occurs from damage to the brain
caused by an outside force, and
may lead to cases of amnesia
depending on the severity of the
injury. Head
injury can
give rise to either transient or
persisting amnesia.
Occasionally, post-traumatic
amnesia (PTA)
may exist without any retrograde
amnesia (RA), but this is often
more common in cases of
penetrating lesions. Damage to
the frontal or anterior temporal
regions have been described to
be associated with
disproportionate RA. Studies
have illustrated that during
PTA, head injury patients showed
accelerated forgetting of
learned information. On the
other hand, after PTA,
forgetting rates were normal.
As noted in the above-mentioned
section on traumatic brain
injury it can be associated with
memory impairment, Alzheimer's
disease; however, as far as
aging is concerned it poses
other threats as well. There is
evidence that supports a high
incidence of falls among the
elderly population and this is a
leading cause of TBI-associated
death among the population of
people 75 years of age and
older.When looking at the chart
to the right on the page, it
states that falls are only 28%
of the total causes of TBI, so
that would suggest that the
elderly make up a good portion
of that 28% overall. Another
factor associated with TBI and
age is the relationship between
when the injury was sustained
and the age at which it
occurred. It is estimated that
the older the individual, the
more likely they would require
assistance post TBI.
In some cases, individuals have
reported having a particularly
vivid memory for images or
sounds occurring immediately
before the injury, on regaining
consciousness, or during a lucid
interval between the injury and
the onset of PTA. As a result,
recent controversy has emerged
about whether severe head injury
and amnesia exclude the
possibility of post-traumatic
stress disorder (PTSD)
symptoms. In a study carried out
by McMillan (1996), patients
reported ‘windows' of
experience, in which emotional
disturbance was sufficient to
cause PTSD. These 'windows'
involved recall of events close
to impact (when RA was brief),
of distressing events soon after
the accident (when PTA was
short), or of 'islands' of
memory (e.g. hearing the
screaming of others).
Brain injuries can also be the
result of a stroke as
the resulting lack of oxygen can
cause damage to the location of
the cerebrovascular accident
(CVA). The effects of a CVA in
the left and right hemispheres
of the brain include short-term
memory impairment, and
difficulty acquiring and
retaining new information.
-
Dementia
Dementia refers
to a large class of disorders
characterized by the progressive
deterioration of thinking
ability and memory as the brain
becomes damaged. Dementia can be
categorized as reversible (e.g. thyroid disease)
or irreversible (e.g.
Alzheimer's disease). Currently,
there are more than 35 million
people with dementia worldwide.
In the United States alone the
number of people affected by
dementia is striking at 3.8
million.
While studies show that there
are “normal” aspects to aging,
such as graying hair and changes
in vision, there are changes
such as forgetting how to do
things that are not considered
“normal”. The importance of
understanding that the changes
most frequently observed and
noticed on a daily basis
concerning aging loved ones is
imperative. While mild cognitive
impairment can be considered a
normal part of aging, the
differences must be noted.
In one study by J. Shagam, it
was noted that while Diabetes
and Hypertension are not
considered part of normal aging,
they would be classified under
mild cognitive impairment.With
this being said, it is important
to differentiate the differences
with what can be potentially
harmful and what is not. It is
difficult to accurately diagnose
dementia due to the fact that
most people are unaware of what
to be looking for and also
because there is no specific
test which can be given as a
diagnostic tool.
What is even more evident is
that the symptoms among
dementia, Alzheimer's and
Parkinson's related dementia
tend to go beyond just one
ailment. While there are
different forms of dementia,
Vascular dementia as it would
sound is associated with
vascular cautions.
This form of dementia is not a
slow deterioration but rather a
sudden and unexpected change due
to heart attack or
stroke significantly reducing
blood to the brain. Research
has shown that persistent
hypertension can be contributory
to the breakdown of the BBB. The
blood-brain barrier (BBB) serves
as a “gatekeeper” for the brain
by keeping out water and other
substances. Various studies show
that as the brain ages the
blood-brain barrier starts to
break down and become
dysfunctional. There are
different ways to measure the
thinning of the BBB and one that
most are familiar with is
imaging, this consists of taking
pictures of the brain using CT
scans, MRI, or PET scans.
Previous research also indicates
that with aging and the thinning
of the BBB, cognitive changes
were also occurring within the
section of the brain known as
the hippocampus. This shows a
relationship between aging and
the thinning of the BBB and its
effects on the brain. Also
indicated by the aging brain are
learning and memory impairments.
While changes to the BBB are not
a cause of impairment to
cognitive functions alone
research suggests that there is
a relationship. Another
impairment which is indicative
of brain aging and the breakdown
of the BBB is the accretion of
iron.
Too much iron in the body can
create free radicals which could
influence the degeneration of
the blood-brain barrier. One
other specific age related
factor noted in Popsecu et al.
is a decrease in estrogen as one
ages could adversely affect the
breakdown of the blood-brain
barrier and create a sensitivity
to neurodegeneration. As pointed
out earlier, dementia is a broad
category of memory impairments
most commonly associated with
ageing. Another symptom which
should be monitored is Type 2
diabetes, which can lead to
vascular dementia.
Also linked with vascular
dementia issues is high
cholesterol; furthermore, this
risk factor is related to
cognitive decline, stroke, and
Alzheimer's disease. It is
estimated that within 20 years,
worldwide prevalence will
increase twofold. By 2050, this
number is expected to increase
to 115 million. Overall,
dementia incidence is similar
for men and women. However,
after 90 years of age dementia
incidence declines in men but
not in women.
-
Hyperthymestic syndrome
Hyperthymestic syndrome
causes an individual to have an
extremely detailed autobiographical
memory. Patients with this
condition are able to recall
events from every day of their
lives (with the exception of
memories before age five and
days that were uneventful). This
condition is very rare with only
a few confirmed cases.
-
Huntington's disease
Huntington's disease (HD)
is an inherited progressive
disorder of the brain that leads
to uncontrolled movements,
emotional instability, and loss
of intellectual
faculties. Because of the
inheritability of Huntington's
each child born to a parent with
Huntington's has a 50% chance of
inheriting the disease, leading
to a prevalence of almost 1 in
10,000 Canadians (0.01%).
The first signs of Huntington's
Disease are generally subtle;
sufferers commonly note tics and
twitching as well as unexplained
fluctuations of mood.
Clumsiness, depression and
irritability are noted. What
begins as a slurring and slowing
of speech eventually leads to
difficulty communicating and
confinement to a wheelchair or
bed.
-
Parkinson's disease
Parkinson's disease (PD)
is a neurodegenerative disease.
PD and aging share a lot of the
same neuropathologic and
behavioral features. Movement is
normally controlled by dopamine;
a chemical that carries signals
between the nerves in the brain.
When cells that normally produce
dopamine die off, the symptoms
of Parkinson's appear. This
degeneration also occurs in
normal aging but is a much
slower process. The most common
symptoms include: tremors,
slowness, stiffness, impaired
balance, rigidity of the
muscles, and fatigue. As the
disease progresses, non-motor
symptoms may also appear, such
as depression, difficulty
swallowing, sexual problems or
cognitive changes.
Another symptom associated with
PD is memory dysfunction. This
can be attributed to frontal
lobe damage and presents itself
in a manner which could be
associated in normal aging.
However, there is no certain
correlation between normal aging
and that of Parkinson's disease
with relation to memory
specifically. According to
studies done in London and in
Sicily, 1 in 1000 elderly
citizens will be diagnosed with
Parkinson's, although this can
vary regionally and affect a
large range of age groups.
Cognitive impairment is common
in PD. Specific parkinsonian
symptoms, bradykinesia and
rigidity, have been shown to be
associated with decline of
cognitive function. The
underlying neuropathological
disturbance in PD involves
selective deterioration of
subcortical structures, and the
executive dysfunction in PD,
especially in processes that
involve working memory. This has
been shown to be related to
decreased activation in the
basal ganglia and frontal
cortex. Elgh, Domellof, Linder,
Edstrom, Stenlund, & Forsgren
(2009) studied cognitive
function in early Parkinson's
disease and found that PD
patients performed significantly
worse than healthy controls in
attention, episodic memory,
category fluency, psychomotor
function, visuospatial function
and in several measures of
executive function. Patients
also exhibited greater
difficulty with free recall that
required a preserved executive
function than with cued recall
and recognition in tests of
episodic memory.
According to a Japanese study,
normal elderly subjects had
difficulty with memory
recognition and the PD elderly
subjects had an even more
troubling time with recognition
than the normal group Another
pertinent correlation made by
this Japanese survey is that for
PD patients their immediate
memory response is intact while
their ability to recognize
memories from the past are
inhibited. It is also said that
PD patient memory is considered
a selective impairment.
-
Stress
It has become clear that aging
negatively affects brain
function and this can encompass
a decrease in locomotor
activities and coordination as
well as affect in a negative way
learning and memory. Certain
responses to stress within the
hippocampus can have negative
effects on learning. In a study
done by Mark A. Smith, it is
demonstrated that exposure to
continuous stress can cause
age-related issues to the
hippocampus. What then becomes
more noticeable is that the
aging brain is not as able to
recognize growth, this is a
symptom of hippocampal damage.
If the information is not being
encoded properly in the brain
then of course there would not
be good memory retention without
the consideration of outside
implications. However, the
consideration of anxiety, memory
and overall function must be
compromised. An emotional memory
is capable of being embedded and
then reused in a similar
scenario at a later time if need
be. Also noted within a study
relating to age and anxiety and
memory it was noted that lesions
on the brain can affect spatial
learning as well as sex
presenting at a disadvantage.
Dysfunction within the
hippocampus can be a reason
behind aging brain changes among
the elderly. To sum up anxiety
and memory and aging, it is
useful to recognize a
correlation between what anxiety
can cause the body to do and how
memories are then formed or not
formed, and how the aging brain
has enough difficulty on its own
trying to perform recall tasks.
-
Wernicke- Korsakoff's syndrome
Wernicke-Korsakoff syndrome (WKS)
is a severe neurological
disorder caused by thiamine (vitamin B1)
deficiency, and is usually
associated with chronic
excessive alcohol consumption.
It is characterized clinically
by oculomotor abnormalities, cerebellar dysfunction
and an altered mental state.
Korsakoff's syndrome is also
characterized by profound
amnesia, disorientation and
frequent confabulation (making
up or inventing information to
compensate for poor memory). A
survey published in 1995
indicated that there was no
connection to the national
average amount of alcohol
ingested by a country in
correlation to a range of
prevalence within 0 and 2.5%.
Symptoms of Wernicke-Korsakoff
Syndrome include confusion,
amnesia, and impaired short-term
memory. WKS also tends to impair
the person's ability to learn
new information or tasks. In
addition, individuals often
appear apathetic and inattentive
and some may experience
agitation. WKS symptoms may be
long-lasting or permanent and
its distinction is separate from
acute effects of alcohol
consumption and from periods of
alcohol withdrawal.
-
Aging
Normal aging,
although not responsible for
causing memory disorders, is
associated with a decline in
cognitive and neural systems
including memory (long-term and
working memory). Many factors
such as genetics and neural
degeneration have
a part in causing memory
disorders. In order to diagnose
Alzheimer's disease and dementia
early, researchers are trying to
find biological markers that can
predict these diseases in
younger adults. One such marker
is a beta-amyloid deposit
which is a protein that
deposits on the brain as we age.
Although 20-33% of healthy
elderly adults have these
deposits, they are increased in
elderly with diagnosed
Alzheimer's disease and
dementia.
Additionally, traumatic brain
injury, TBI, is increasingly
being linked as a factor in
early-onset Alzheimer's disease.
One study examined dementia
severity in elderly schizophrenic patients
diagnosed with Alzheimer's
disease and dementia versus
elderly schizophrenic patients
without any neurodegenerative
disorders. In most cases, if
schizophrenia is diagnosed,
Alzheimer's disease or some form
of dementia in varying levels of
severity is also diagnosed. It
was found that increased
hippocampal neurofibrillary
tangles and
higher neuritic plaque density
(in the superior temporal gyrus,
orbitofrontal gyrus, and the
inferior parietal cortex) were
associated with increased
severity of dementia. Along with
these biological factors, when
the patient also had the apolipoprotein
E (ApoE4) allele (a
known genetic risk factor for
Alzheimer's disease), the
neuritic plaques increased
although the hippocampal
neurofibrillary tangles did not.
It showed an increased genetic
susceptibility to more severe
dementia with Alzheimer's
disease than without the genetic
marker.
As seen in the examples above,
although memory does degenerate
with age, it is not always
classified as a memory disorder.
The difference in memory between
normal aging and a memory
disorder is the amount of
beta-amyloid deposits,
hippocampal neurofibrillary
tangles, or neuritic plaques in
the cortex. If there is an
increased amount, memory
connections become blocked,
memory functions decrease much
more than what is normal for
that age and a memory disorder
is diagnosed.
The cholinergic hypothesis of
geriatric memory dysfunction is
an older hypothesis that was
considered before beta-amyloid
deposits, neurofibrillary
tangles, or neuritic plaques. It
states that by blocking the cholinergic mechanisms
in control subjects you can
examine the relationship between
cholinergic dysfunction and
normal aging and memory
disorders because this system
when dysfunctional creates
memory deficits.